Abstract
Introduction: Age-adjusted incidence and mortality rates for multiple myeloma (MM) have been higher among Blacks/African Americans (AAs) than Whites in the United States. Yet several prospective and real-world retrospective studies have suggested similar, or even improved, outcomes among Blacks/AAs, particularly when there is equal access to care. Real-world (RW) evidence can provide important insight into factors that impact patient (pt) outcomes in everyday practice. This retrospective, observational cohort study sought to describe associations between pt, disease, and treatment characteristics and survival outcomes by race/ethnicity.
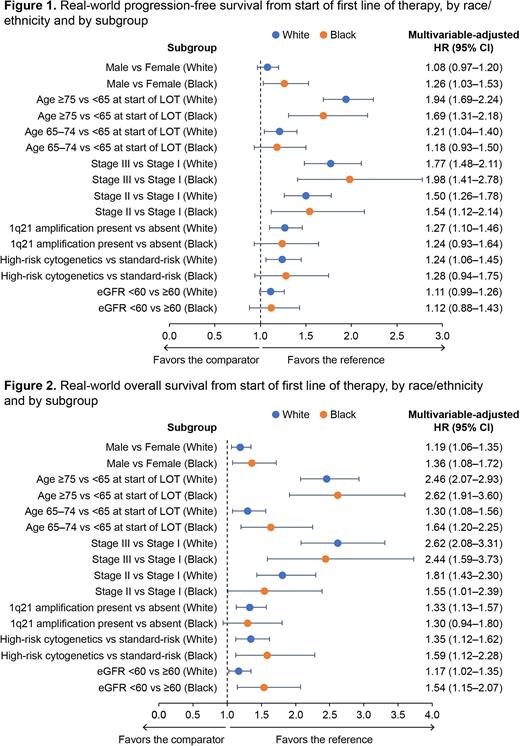
Methods: This study used the nationwide Flatiron Health electronic health record-derived, de-identified database of MM pts treated in the United States. During the study period of January 1, 2016, to January 31, 2022, pts whose first-line treatment was initiated after the study start date and whose race/ethnicity was categorized as either non-Hispanic (NH) White or NH Black/AA were included. Pts with evidence of treatment >14 days prior to their diagnosis date were excluded. We examined pt, disease, and treatment characteristics by race/ethnicity. We also examined RW progression free-survival (rwPFS) and overall survival (rwOS), indexed to first line of therapy (LOT). rwPFS was defined as the time from start of first LOT to the date of first progression event (informed by International Myeloma Working Group criteria and incorporating both abstracted M spike values and structured free light chain values) or death. rwOS was defined as the time from start of first LOT to the date of death. Differences in rwPFS and rwOS were assessed using the Kaplan-Meier method. Multivariable (MV) Cox proportional hazards models were used to examine associations between pt, disease, and treatment characteristics and outcomes by race/ethnicity.
Results: At the time of data cutoff, 4387 pts had initiated first LOT; 1017 (23.2%) were Black/AA and 3370 (76.8%) were White. The median age at both MM diagnosis and start of first LOT was 68 years among Black/AAs and 71 years in Whites. Black/AAs were more likely than Whites to be female (53.0% vs 43.6%) and from the Southern United States (64.1% vs 36.3%). Rates of high-risk cytogenetics and 1q21 amplification were similar between races/ethnicities, as was median time from MM diagnosis to start of first LOT. Most Blacks/AAs (53.6%) and Whites (53.4%) received a proteasome inhibitor/immunomodulatory drug-based regimen as first LOT; Black/AA pts were less likely to receive stem-cell transplant than Whites (16.7% vs 21.8%). In unadjusted analyses indexed to first LOT, median rwPFS (25.4 vs 26.7 months) and median rwOS (64.6 vs 59.7 months) were similar for the overall populations of Black/AAs and Whites, respectively. MV-adjusted analyses examining associations between selected variables and outcomes by race/ethnicity are shown in Figure 1 (rwPFS) and Figure 2 (rwOS). Age of ≥75 at start of first LOT (compared to age of <65 years), Eastern Cooperative Oncology Group Performance Status (PS) of 2 (compared to PS of 0) and International Staging System Stage II or III disease at diagnosis (compared to Stage I disease at diagnosis) were associated with statistically inferior rwPFS and rwOS for both Black/AAs and Whites. The presence of high-risk cytogenetics or 1q21 amplification (compared to standard-risk cytogenetics or absence of 1q21 amplification, respectively) were similarly associated with worse rwPFS among both Black/AAs and Whites, though were only statistically significant among Whites. The presence of high-risk cytogenetics was significantly associated with worse rwOS among both races/ethnicities. 1q21 amplification was similarly associated with worse rwOS in both subgroups but was not statistically significant among Black/AAs.
Conclusions: Among RW pts with MM from the Flatiron Health database, unadjusted rwPFS and rwOS were similar between NH Black/AA pts and NH White pts, as previously reported. In general, associations between risk factors for rwPFS and rwOS were consistent between races/ethnicities. Findings from this study compliment knowledge gained from earlier prospective and RW retrospective studies, helping to inform clinicians about the impact of race/ethnicity on disease characteristics and treatment patterns in the United States as well as MM outcomes within diverse populations.
Funding: Sanofi.
Disclosures
Salinardi:Sanofi: Current Employment, Current holder of stock options in a privately-held company. Rice:Sanofi: Current Employment, Other: may hold stock and/or stock options with Sanofi.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal